Understanding Venous Stasis Causes: A Comprehensive Guide
Venous stasis is a medical condition characterized by poor blood circulation in the lower extremities. It can lead to various complications, such as blood clots, swelling, and varicose veins. Understanding the causes of venous stasis is crucial for effective prevention and treatment. This article will delve into the factors contributing to venous stasis, its implications on health, and provide actionable insights for management.
What is Venous Stasis?
Venous stasis occurs when blood flow in the veins is impaired, particularly in the legs. The veins carry deoxygenated blood back to the heart, and when this process is disrupted, it can lead to various health issues. Venous stasis is often associated with chronic venous insufficiency (CVI), a condition where the valves in the veins fail to function properly.
Common Venous Stasis Causes
1. Prolonged Immobility
One of the leading causes of venous stasis is prolonged immobility. This can occur during long flights, extended hospital stays, or sedentary occupations. When a person remains in one position for too long, the flow of blood in the veins slows down.
2. Obesity
Excess body weight places additional pressure on the veins of the legs, hampering adequate blood flow. Obesity is a significant risk factor for developing venous stasis, as the overweight condition can lead to increased venous pressure, resulting in stasis.
3. Age
As people age, the strength and elasticity of their veins decrease. This can lead to poor circulation and increased susceptibility to venous stasis. Older adults are particularly at risk due to the general decline in vascular health over time.
4. Genetics
Family history can play a vital role in the likelihood of developing venous stasis. Genetic predisposition may lead to inherited conditions affecting the veins, such as hereditary venous insufficiency or connective tissue disorders.
5. Hormonal Changes
Hormones significantly influence blood vessel function. Women, especially during pregnancy, menopause, or while using hormonal contraceptives, may experience changes in blood flow and increased risk of venous stasis due to hormonal fluctuations.
6. Medical Conditions
Several medical conditions can contribute to venous stasis, including:
- Heart failure
- Diabetes
- Varicose veins
- Thrombosis (blood clots)
These diseases can impair the efficiency of the cardiovascular system, leading to stagnation of blood and increased risks of complications.
Symptoms of Venous Stasis
Individuals suffering from venous stasis may experience various symptoms, including:
- Swelling in the lower legs
- Pain or aching in the legs
- Skin discoloration
- Varicose veins
- Ulcers or sores on the skin
If you experience these symptoms, it is vital to consult a healthcare professional for evaluation and potential treatment.
Preventing Venous Stasis
Preventing venous stasis is essential for maintaining vascular health. Here are some effective strategies for reducing the risks associated with this condition:
- Stay Active: Regular physical activity promotes blood circulation. Simple exercises like walking or leg lifts can significantly help.
- Maintain a Healthy Weight: Keeping your body weight in check reduces the pressure on your veins.
- Elevate Your Legs: Elevating your legs periodically can enhance blood flow back to the heart.
- Avoid Prolonged Sitting or Standing: Take breaks to move around, especially during long travel or while at work.
- Wear Compression Stockings: These special stockings help compress the leg veins, promoting better blood flow.
Treatments for Venous Stasis
If venous stasis occurs, various treatment options are available. The choice of treatment will depend on the severity of the condition and individual health factors. Common treatments include:
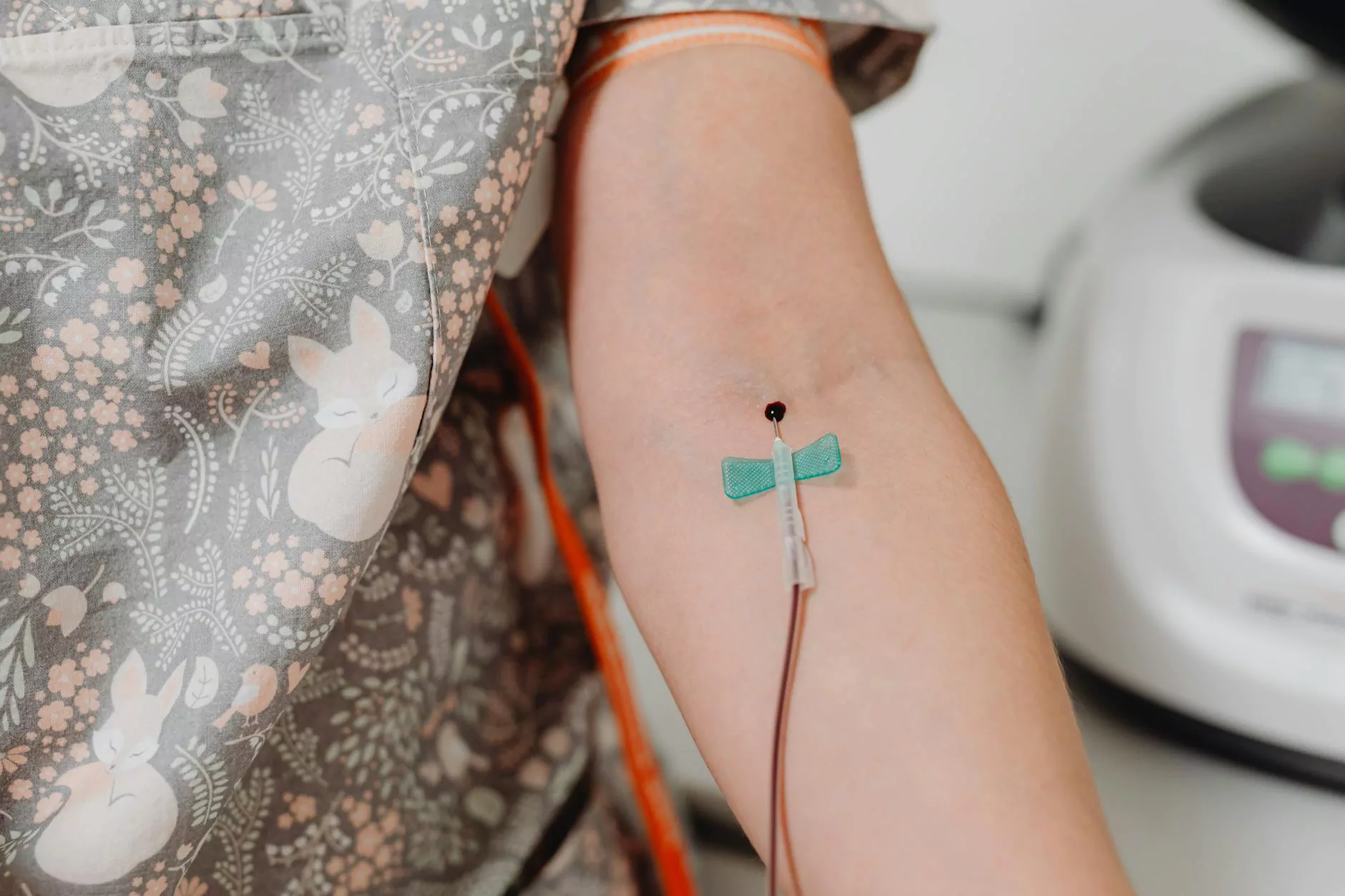
- Medications: Anticoagulants may be prescribed to prevent blood clots.
- Compression Therapy: This involves wearing compression stockings to encourage better blood flow.
- Endovenous Laser Treatment (EVLT): This minimally invasive procedure uses laser energy to close off problematic veins.
- Surgery: In severe cases, surgical options may be necessary to remove or repair veins.
The Role of Vascular Medicine
Vascular medicine specializes in the diagnosis and treatment of vascular conditions, including venous stasis. Vascular specialists use a range of diagnostic tools, including ultrasound examinations, to assess blood flow and identify underlying issues. Early detection and intervention are critical in managing venous stasis effectively.
Conclusion
Understanding the causes of venous stasis is integral to prevention and treatment. By addressing risk factors like immobility, obesity, and underlying health conditions, individuals can significantly reduce their chances of experiencing this condition. Regular check-ups with vascular specialists can help catch any issues early, ensuring appropriate management and maintaining overall vein health.
For more information on venous stasis and vascular health, visit Truffles Vein Specialists.